INTRODUCTION
In February 2011, a 6.3 magnitude earthquake shook the foundations of Christchurch, forcing the evacuation of Canterbury University and the conversion of traditional face-to-face learning to online education (Todorova & Bjorn-Andersen, 2011). In New Orleans, a turbulent hurricane forced Southern University to transform itself into an e-learning campus (Omar et al., 2008). These disasters shifted the traditional pedagogy of in-person classroom teaching to online methods (Kauppi et al., 2020). The evolving nature of the COVID-19 pandemic and restriction policies resulted in nursing faculty across the globe adopting innovative strategies to ensure the delivery of theoretical and practical content (Nashwan et al., 2020). The willingness of nursing faculty to disseminate the initial findings of their innovations has resulted in the rapid publication of COVID-19 literature (Bagdasarian et al., 2020). However, the increasing number of published studies makes it daunting for nurse educators and the research community to access synthesised, up-to-date evidence.
To date, researchers have synthesised evidence on the impact of COVID-19 on the mental health, well-being, and coping strategies of nursing students (Barrett & Twycross, 2022; Keskin & Özkan, 2021; Majrashi et al., 2021). Other systematic reviews reported the efficacy of blended learning (Jowsey et al., 2020), challenges in online learning (Divya & Binil, 2021), and perceptions of e-learning (Alosta & Khalaf, 2021). While these reviews sufficiently document students’ interaction with specific technology and the impact of COVID-19 in general, to our knowledge, no study has synthesised innovations deployed by nursing education in response to the pandemic. With several changes in nursing education during the pandemic (Moreno-Sánchez et al., 2022), nurse educators risk information overload if the emerging innovations are not synthesised.
We aimed to identify the teaching, assessment, and other educational innovations developed in response to the pandemic within nursing education. We chose a scoping review to address this aim, as this methodological tool is considered ideal for a comprehensive understanding of the scope, trends and characteristics of emerging evidence, such as changes in nursing education triggered by the ongoing COVID-19 pandemic (Armstrong et al., 2011; Munn et al., 2018). This scoping review answered these questions: 1) what innovations, improvements or changes in nursing education have been deployed in response to the COVID-19 pandemic; 2) what lessons have been learned from the deployed innovations and changes; and 3) how can these be applied to future educational interventions?
METHODS
The scoping review followed the Arksey and O’Malley (2005) methodology, refined by Levac et al. (2010) and the Joanna Briggs Institute (JBI) (Peters et al., 2017). We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analysis Statement for Scoping Reviews (PRISMA-ScR) recommendations (Tricco et al., 2018).
Review question, inclusion, and exclusion criteria
The eligibility criteria were established a priori and informed by the population-concept-context approach recommended by JBI (Peters et al., 2017). The population of interest were nursing students and faculty members in undergraduate, graduate, and continuing nursing education. The concepts of interest were innovations, improvements, or changes in nursing education in the context of the pandemic. We included published literature of any design type (case reports, case-control studies, editorials, commentaries, letters) due to the emerging nature of the identified innovations, the recency of the pandemic and the lack of class 1 evidence. We limited our search to publications written in English and addressed our question from 1st December 2019 to 31st December 2021. We excluded literature whose primary focus was not nursing students or nursing faculty.
Search strategy
We searched MEDLINE (PubMed), Embase and CINAHL databases to identify titles and abstracts. We developed a comprehensive search strategy with term combinations relating to ‘COVID-19’ and ‘nursing education’. Search terms were adapted from the National Institute for Health and Care Excellence (Levay & Finnegan, 2021). Additional search terms included nursing students, undergraduate, postgraduate, and pre-licensure. The detailed search strategy can be found in Table 1. Additionally, we searched the reference list of included articles to identify literature not indexed in the databases listed above.
Study selection
Identified records from databases were imported into Endnote X9 (Clarivate Analytics, PA, USA) for duplicate removal. Non-duplicate articles were uploaded into Rayyan QCRI (Ouzzani et al., 2016). Rayyan QCRI enables authors to collaborate on the title/abstract screening phases of the review process. Using the ‘blind’ function of Rayyan, two reviewers (CPA and AP) independently screened the same titles and abstracts to determine their relevance for inclusion based on the eligibility criteria. Disagreements were resolved through discussion and consensus. Articles excluded by both authors and confirmed by a third author (IA) were left out of the full-text screening. Where CPA and AP could not resolve discrepancies, a fourth reviewer (CH) acted as a tiebreaker.
Data extraction
We extracted information on the author, date, study type, country, educational level, and sample characteristics. To describe deployed innovations, we extracted data on the type of change undertaken, the technology used, the nature of the intervention and the outcomes. Authors CH and IA randomly crosschecked approximately 10% of the extracted data to ensure accuracy. Identified discrepancies were resolved through discussion.
Data synthesis
Due to the nature of the review (scoping), we did not assess the methodological quality of the primary literature. Instead, we grouped and described conceptual categories narratively due to the heterogeneity of included literature.
RESULTS
Search results
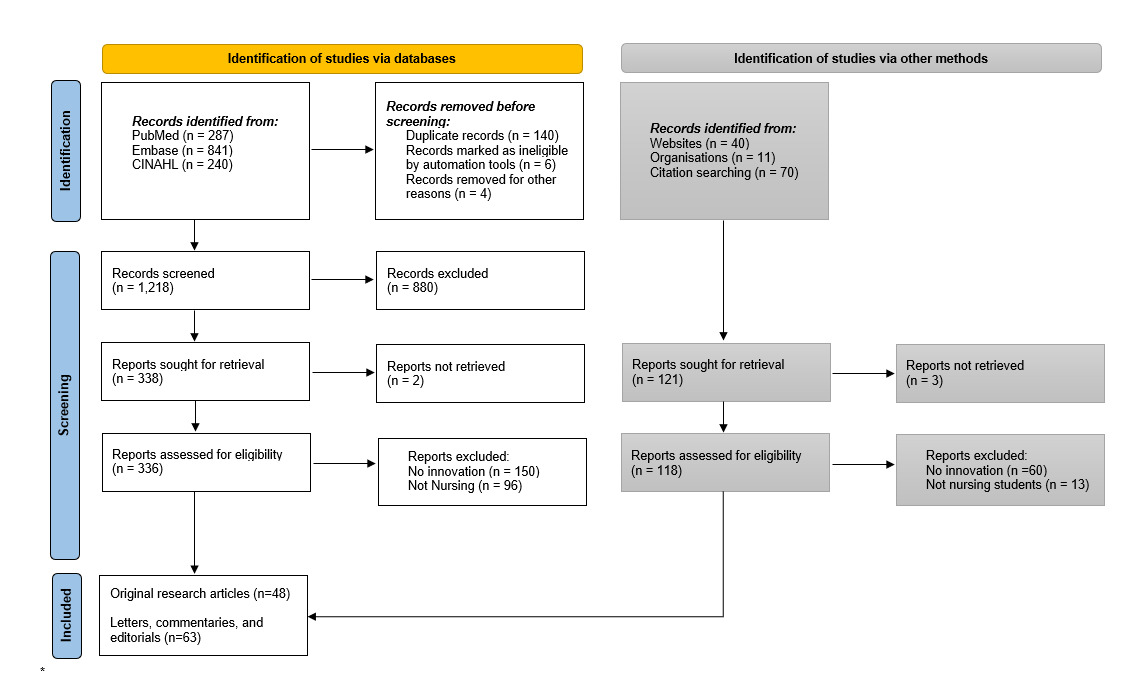
We identified 1339 potentially relevant records of published literature. We excluded articles at various screening stages, as summarised in Figure 1, resulting in 48 full-text articles and 63 editorials, commentaries, or letters.
Characteristics of included literature
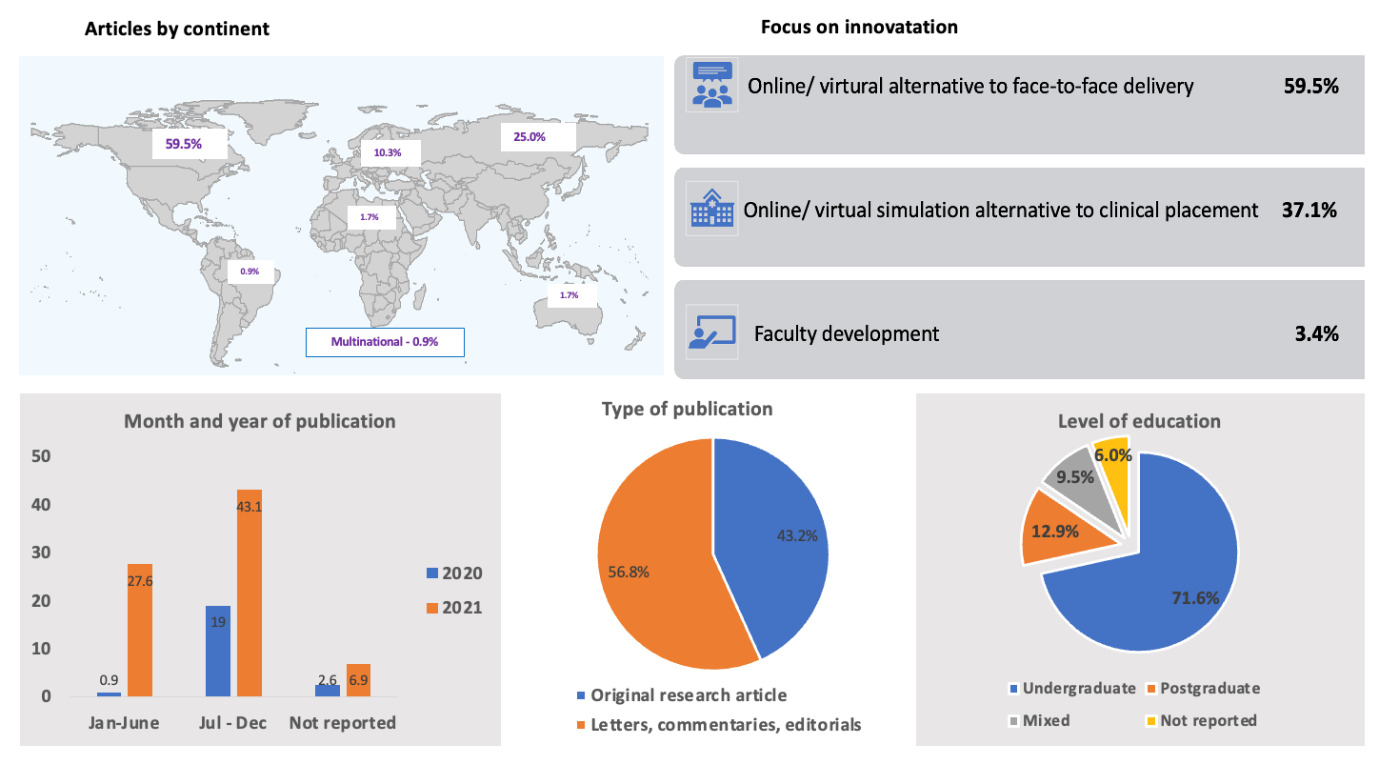
Figure 2 summarises the characteristics of included literature. Forty-eight (43.3%) studies were original research articles, while 63 (57.0%) were letters, commentaries, and editorials. Of all the literature published, 69 (59.5%) were from North America; 29 (25%) from Asia; 12 (10.3%) Europe; and just six from other continents, including two from Africa. Most of the literature was from 2021 with 71.6% relating to undergraduate nursing students and 12.9% to postgraduate.
Aotearoa New Zealand focused literature
Before submitting this manuscript, a focused search of the Aotearoa New Zealand literature identified two studies that were either missed by our broad search strategy (Thomson et al., 2021) or published after the last search had been carried out (Brownie et al., 2022). These studies have been summarised separately in the Supplementary Table, and their implications are explored in the discussion section. Thomson et al. (2021) reported on an innovative, collaborative virtual clinical placement in the primary healthcare setting, while Brownie et al. (2022) evaluated the rapid response to student telehealth experience when implementing interRAI assessments among community-dwelling frail older adults.
Summary of educational innovations
Of the literature reviewed 111 described educational innovations deployed to mitigate the impact of the pandemic. These focused on three areas: 1) online teaching as an alternative to face-to-face delivery (n=69; 59.5%); 2) providing an alternative to clinical placement (n=43; 37.1%); and 3) faculty development (n=4; 3.4%), as shown in Figure 2.
Teaching online as an alternative to face-to-face delivery
Table 2 summarises characteristics of the literature that reported substituting face-to-face teaching with some form of online learning (n=37; 53.6%), virtual simulation (n=26; 37.7%) or both (n=6; 8.7%). This literature originated from North America (33;47.1%) and Asia (22; 31.4%). The majority (56; 81.2%) focused on the undergraduate nursing population. All the literature (4; 5.8%) involving postgraduate nursing students came from North America. Papers described delivering teaching content synchronously (28; 40.6%), asynchronously (5; 7.2%) or both (11; 15.9%). The approach to delivery was not clear in 11 (15.9%) of the articles.
Online learning environment
Transitioning to an online learning environment was crucial for the continued functioning of nursing programmes. This included modified traditional teaching to allow for online assessment (n=4); student engagement with course content (n=7); and capacity-building in the care of COVID-19 patients (n=2). Online assessment strategies included modifications to traditional objective structured clinical examination (OSCE) for simulated online scenarios (Arrogante et al., 2021; Bradford et al., 2021), collaborative role plays (A. Miller & Guest, 2021), and self-recorded demonstration of skill proficiency (Palmer et al., 2021). Bradford et al. (2021) used a scripted scenario and actor patient to simulate telehealth experiences while assessing women’s health nurse practitioners’ knowledge, clinical reasoning, and professional behaviours. Many authors identified prompt feedback as challenging (Puljak et al., 2020). However, they all agreed that the approach could be extended to normal situations, even after pandemics.
The use of blended (n=3) and flipped learning strategies (n=4) were reported to improve learner engagement. Ropero-Padilla et al. (2021) developed a blended learning approach with game elements for two undergraduate nursing subject areas to support teaching key clinical or teamwork-related skills such as creativity, innovation, team-based communication, and responsibility. Other literature included in this review have demonstrated that a flipped classroom combined with a game-based interactive learning platform (Chan et al., 2021) and jigsaw methods improved student engagement and motivation during online sessions. Other student engagement strategies included Zoom breakout rooms (n=3), small groups work (Gedney-Lose, 2021), a lab for home visiting (DeGroot et al., 2021) and a simulation suite (Cowperthwait et al., 2021).
Two studies described innovative approaches adopted to enhance the learning capacity of nursing students and faculty in the management of COVID-19. Tyerman et al. (2021) described a virtual simulation game educational module focused on COVID-19 assessment and personal protective equipment to strengthen graduating nursing students and practising nurses’ capacity to provide care during the surge in COVID-19 cases. Prata et al. (2020) promoted collaborative learning of knowledge about COVID-19 among nursing graduates at a public university in Rio de Janeiro.
The majority (51.4%) of the literature did not report the technology used to deliver the online intervention. Only 12 (32.4%) articles specified the content delivered online, and this included public health (n=4), biological science (n=3), disease process (Joshi et al., 2021; Langegård et al., 2021), evidence-based practice (Svoboda & Stevenson, 2021), and foundational nursing (Chan et al., 2021; Scheller et al., 2021) related content.
Virtual simulation
Substitution of classroom skill training with virtual simulation experiences was a significant educational development to address the impracticalities and intensive staffing requirements of classroom-based clinical simulation during COVID-19. Of the included literature, 27 (38.6%) described the integration of virtual simulation experiences into nursing programmes using various technologies, including Zoom, a three-dimensional learning management system, Microsoft Teams and 360 images. Skill development within the virtual simulated experience focused on vital sign recording (Ansell & Whitehead, 2021), health assessment activities (Aul, 2020; Keller & Spangler, 2021), discharge planning (Wen et al., 2021), and intramuscular injection administration (Khraisat et al., 2020). Jiménez-Rodríguez et al. (2020) used simulated nursing video consultation to augment an existing clinical practicum course. Gibson et al. (2021) described the development of a telehealth curriculum that included interactive videos and simulated clinical experiences.
Alternative to clinical placement
Clinical placement for nursing students was significantly disrupted during the pandemic, requiring alternative ways to provide clinical learning experiences. Forty-three papers (37.1%) described substituting clinical placement with other teaching and learning experiences for undergraduate (27; 63.5%), postgraduate (10; 23.3%), or both undergraduate and postgraduate (3; 7.0%) nursing students. Twelve papers (27.9%) described using telehealth technology to create alternative clinical spaces (6; 14%) and virtual simulation sessions (5; 11.6%). Most literature (31; 72.1%) reported using other virtual learning platforms to assist with skill assessment (4; 9.3%), help students solve case studies (6; 14.0%), and undertake virtual simulation sessions (21; 48.8%). Close to half of these interventions were delivered synchronously (20; 46.5%), but this was unclear in 3.4% of the papers (Table 3).
Telehealth technology to create alternative clinical spaces and simulation sessions
Six reported on innovative approaches used to help undergraduate (Jiménez-Rodríguez & Arrogante, 2020) and postgraduate nursing students attain alternative forms of clinical experience after the abrupt closure of usual clinical sites (Table 3). Authors relied on Zoom (n=3) and other telehealth technologies to deliver clinical teaching content. LaManna et al. (2021) used Telehealth Robotic Technology with standardised actor patients to develop a formative simulated telehealth visit and deliver gerontologic scenarios. Winship et al. (2020) developed a hybrid telephone-based programme to provide interprofessional training experiences to enable nurse practitioner students to complete their clinical hours.
Authors used telehealth technology to synchronously deliver simulation sessions to undergraduates (n=3) and a combination of postgraduate and undergraduate (Fogg et al., 2020; Gedney-Lose, 2021) nursing students. The simulation sessions focused on client assessment (DeFoor et al., 2020), creation of evidence-based guidelines (Fogg et al., 2020), cardiovascular risk assessment (Gedney-Lose, 2021), and debriefing sessions (Fung et al., 2021).
Virtual platform for skill assessment, case studies, and virtual simulation
Virtual platforms were used to assess student clinical skills (4; 9.3%), deliver case studies (6; 14.0%) and simulation sessions (21; 48.8%). Four used virtual platforms to assess the clinical skills of postgraduate (Fraino & Selix, 2021; Jones et al., 2021), undergraduate (Nugroho & Prihanto, 2021), or both (Badowski et al., 2021). Only Jones et al. (2021) used synchronous and asynchronous approaches for the assessment.
Six papers described the virtual delivery of synchronous and asynchronous case studies in place of clinical hours to postgraduate (Callender et al., 2021) and undergraduate (n=5) students. The synchronous delivery of case studies offered a realistic clinical setting (Callender et al., 2021) and the opportunity to examine determinants of health without direct contact with the communities (Bejster et al., 2021). For example, Tracy and McPherson (2020) used synchronous virtual technologies to deliver an unfolding case study that included the COVID-19 pandemic and applied real-life situations to students’ current clinical placements. Kubin et al. (2021) utilised an online platform to present unfolding case studies covering various paediatric disorders. Although these approaches could not replace direct patient care, the authors reported improved student engagement, retention, and clinical judgement.
Twenty-one papers described replacing onsite clinical placement with virtual simulation opportunities. Four of these employed both synchronous and asynchronous approaches to enable students to undertake client assessments (DeFoor et al., 2020), offer community support services (Gresh et al., 2021), and improve student competence and learning experiences (A. Miller & Guest, 2021; Peachey et al., 2021). Five used synchronous virtual simulation to incorporate debriefing sessions (n=3) and facilitate clinical learning and simulation experience (Kim et al., 2021; Kubin et al., 2021). Simulation sessions with innovative digital escape rooms and case studies increased students’ clinical reasoning and prioritisation skills (Kubin et al., 2021). Simulation sessions with virtual simulation enabled learners to make sense of learned content (Dreifuerst et al., 2021) and provided realistic clinical experiences while meeting their learning needs (Fung et al., 2021). Literature that included debriefing sessions showed that excluding debriefing sessions limited students learning outcomes (Dreifuerst et al., 2021) and that best practice in-person debriefing guidelines may not address the nuances of the synchronous virtual environment (Goldsworthy & Verkuyl, 2021).
Faculty development
Four papers reported faculty support programmes (Burton et al., 2021; Howe et al., 2021; Sanford et al., 2021; Swaminathan et al., 2021). Two focused on supporting nursing faculty as they pivoted to online education in response to the pandemic. These included an online course to support faculty staff (Burton et al., 2021) and nurse educators’ competencies in creating and delivering online content (Swaminathan et al., 2021) and transitioning in-person interviews for a baccalaureate programme into a virtual environment (Sanford et al., 2021).
DISCUSSION
This scoping review aimed to identify innovative improvements or changes in nursing education developed by nursing faculty in response to the COVID-19 pandemic globally. The 111 papers published between 2020 and 2021 reported a rapid conversion of in-person classroom teaching and clinical placement models into some form of remote or online learning. Traditionally, health science courses, including nursing, have been delivered mainly through face-to-face in-person activities and clinical placement that allow students to observe and learn from experienced nurses (Bleakley, 2002). Online or e-learning only served as an add-on to fully implemented face-to-face teaching (Fauzi, 2022). Traditional classroom learning was recently preferred, as it fostered learner-tutor and student-student interactions (Kunin et al., 2014). The increase in technology in the past decade and the burgeoning demand for engaging large groups of students at one time have gradually increased the use of online learning platforms (Kauppi et al., 2020; Sinclair et al., 2015). It is not surprising that nursing schools found the online space and its pedagogical practices as the most suitable alternative for ensuring the continuity of academic activities during the pandemic (Barron et al., 2021).
It is important to distinguish between studies that reported remote teaching and clinical placement activities that would be in person were it not for the COVID-19 pandemic and the carefully designed and thoroughly thought through online teaching. Many of the identified innovations in this scoping review may best be described as temporary solutions to the immediate problem of the COVID-19 pandemic and therefore do not constitute well-planned online learning or teaching. Being aware of the differences, Hodges et al. (2020) proposed the term emergency remote teaching to describe the temporary shift of instructional delivery to remote learning. Although the purpose of emergency remote teaching is not to replace the tested and robust in-person pedagogical practices, there is potential for it to become an alternative traditional learning space in emergencies. The innovations reported in this review contribute to our understanding that traditional classroom and clinical placement learning activities do not translate into remote or online learning, hence the variety of pedagogical adaptations reported by nursing faculty across the globe.
It is also evident in this review that nursing faculty made several pedagogical changes and redesigned courses overnight without institutional support. This experience may be particularly stressful for nursing faculty with limited experience in online delivery (Bao, 2020; Didenko et al., 2021; Hodges et al., 2020). Before the pandemic, campus IT supported and trained a relatively small pool of faculty who taught online. Transitioning unexpectedly from in-person to remote teaching across entire campuses might have stretched the support staff and prevented them from offering the same level of support to all the faculty (Nabolsi et al., 2021). The nature of institutional support and how to meet them during pandemic situations needs further exploration. Providing institutional support even during the pandemic crisis would prevent the risk of nursing faculty replicating face-to-face content within the online learning domain without modification or adaptation (Iheduru-Anderson & Foley, 2021).
The restrictions imposed by the pandemic were associated with synchronous and asynchronous simulation instead of in-person teaching by faculty staff. Our review identified virtual simulation as an innovative tool employed by faculty to deliver virtual learning, for example, teaching students new education content as part of the course’s theoretical components and as a substitute for clinical placement hours. Simulation has proven beneficial for nursing education and has shown equivalency with traditional clinical placement relating to skills, knowledge, and confidence (Bradford et al., 2021; Diaz & Walsh, 2021; Peisachovich et al., 2022). Understandably, the abrupt substitution of simulation for clinical placement meant that many articles did not report on details such as the equivalency of substituted hours. Other practical issues previously identified (Bagdasarian et al., 2020) and reflected in this review provide inadequate details on the level of faculty training, simulation modalities, and debriefing methods.
Substituted virtual simulation for clinical placement hours and face-to-face classroom teaching was reported in much of the literature. What remains unknown is whether virtual simulation provides adequate student learning and development of clinical competencies. Before the pandemic, there was no consensus among various nursing regulatory bodies on the ideal balance between simulation and clinical practice hours (Roberts et al., 2019). This was attributable to the vast differences in the required clinical hours worldwide (E. Miller & Cooper, 2016; Roberts et al., 2019). For example, in the United States, clinical hours vary from state to state, with no minimum hours stipulated by the regulatory boards (Hungerford et al., 2019). Replacing clinical hours and face-to-face teaching with simulation requires regulation to ensure uniformity in nursing education standards. Thomson et al. (2021) received approval from the Nursing Council of New Zealand to design an innovative clinical placement alternative in primary healthcare settings when Bachelor of Nursing students in Aotearoa New Zealand could not complete their clinical placement due to COVID-19 restrictions. It will be valuable to gain further insight into how these innovative approaches inform the design of clinical practice curricula. We found that nursing faculty and other interdisciplinary teams could successfully use telehealth to create alternative spaces for clinical skill acquisition during a pandemic. Telehealth has previously been used to provide multiple components of clinical care (Doraiswamy et al., 2020) and case discussion in residency training (Denning et al., 2020). During the pandemic, telehealth guided and engaged students to perform focused assessment, medication management, and pain management activities. More rigorous research is needed to understand and mitigate associated challenges to ensure the prudent use of telehealth.
Learner engagement approaches such as blended learning and breakout rooms, which allowed small group discussions, were crucial to establishing knowledge acquisition in the online environment. However, many papers only described moving face-to-face teaching content online without describing modifications to ensure engagement. Online content and face-to-face teaching are different, and therefore replicating in-person teaching without the necessary modification can be problematic. Factors that influence student engagement in online learning platforms during the crisis have been described elsewhere (Khlaif et al., 2021). It is expected that even after the COVID-19 pandemic, online delivery will become an integral part of nursing education. Therefore, the issue of student engagement needs critical attention.
While much of the included literature demonstrated novel and promising innovative pedagogical strategies in response to the pandemic, very few have examined the impact of these innovations. For example, only 3.4% of articles included reported outcomes, such as change in student behaviours; instead, literature reported on student reaction or perception (47.4%) of the innovations. Similar trends have been observed in reviews that examined adaptations to other health worker education during the pandemic (Khoshrounejad et al., 2021; Park et al., 2021). Reporting these interventions without appropriate outcome and impact measures may impede their expansion (Khoshrounejad et al., 2021). Future studies must objectively collect outcome and impact data (Ng, 2021). Such data may include evaluating the competencies of newly graduated registered nurses who experienced the shift to online learning. Longitudinal studies examining the performance of nursing students during the COVID-19 pandemic are also needed (Goni-Fuste et al., 2021).
Strengths and limitations
The findings and conclusions drawn from this review are robust. We rigorously employed a well-developed and expanded query. However, our study should be interpreted with the following limitations in mind. Considering the diversity of COVID-19 related research and the relevance of the emerging digital pedagogies, we included all papers that provided summaries of ongoing interventions. While the approach ensured comprehensive coverage, many papers provided inadequate detail of interventions and outcomes. Because of this, and in line with the scoping review’s methodology, we did not assess the quality of included articles. Evidence suggests that the quality of these COVID-19 related papers is low (Balaphas et al., 2020). As most studies were conducted in the undergraduate pre-registration nursing population, it limits the generalisation of our results to the entire nursing student population.
Implications for nursing education and research
Our finding has several implications for nursing practice and research in Aotearoa New Zealand and beyond. The two studies from Aotearoa New Zealand (Brownie et al., 2022; Thomson et al., 2021), and the new nursing standards issued by the Nursing Council of New Zealand (2019) to mitigate COVID-related clinical placement challenges, point to ongoing innovative activities in response to the COVID-19 pandemic. The described innovations from this scoping review have replicable components for local contexts. International literature and evidence from Aotearoa New Zealand provide valuable knowledge worthy of further examination even after the global emergency has passed. The review points to the need for nursing faculty to consider a structured approach to introducing new approaches into nursing education by relying on theories of learning and other established pedagogical principles. Finally, nursing faculty’s flexibility and resilience to continue offering nursing education with modified arrangements are evident in this review. Implicit in this success story is the realisation that nurse educators need to be upskilled to deliver effectively in the new platforms described. There is a need for process evaluation data to examine the faculty development features that contribute to teacher performance changes. In addition, studies should focus on the sustainability and effectiveness of these innovations in the post-pandemic period. There is a need to assess the impact of faculty development on the institution/organisation more rigorously and systematically.
CONCLUSION
Our scoping review highlights unprecedented nursing educational changes implemented in response to the COVID-19 pandemic. The move to synchronous and asynchronous online learning and simulations ensured uninterrupted teaching and allowed nursing academics to embrace new pedagogies. This transformed delivery of nursing education is expected to persist even after the pandemic. Attention must be paid to faculty development and support, learner engagement, and the long-term effectiveness of innovations. Further studies are required in assessment and faculty development to sustain quality and impactful nursing education.
Funding
None
Conflicts of interest
None